Introduction
Acute myeloid leukemia (AML) has been considered as a hematological emergency. However, debates on how much the time from diagnosis to treatment (TDT) can be justified to choose the optimal treatment in AML have been raised due to the increased possibility of customized treatment with novel targeted agents based on genetic abnormalities tested by newly applicable diagnostic tools. Three recent studies with a large data set from Western countries showed conflicting results about the relationship between TDT and prognosis. Thus, we evaluated the influence of TDT on patients' outcomes from a large data set of Asian patients.
Methods
We retrospectively evaluated a cohort of AML patients aged 18 and older who visited the Catholic Hematology Hospital in Korea and received anthracycline-based intensive chemotherapy from 2002 to 2016. A total of 1313 patients were included in this analysis, of which 1282 were used for analysis, excluding 26 patients with incomplete documentation and with more than 90 days of TDT. Patients under the age of 60 (Young group, YG) and patients over 60 years of age (Elderly group, EG) were analyzed as an individual cohort. In both cohorts, the effects of TDT on complete remission (CR/CRi), early death (ED), and overall survival (OS) were analyzed. The TDT was analyzed as a continuous variable to minimize the loss of information, while also grouped into four ordinal groups of 1-5, 6-10, 11-15, and 16- to visualize data and find appropriate cutoff. In order to adjust for the influence of established prognostic variables on the outcomes, we used multivariate regression models. In both univariate and multivariate analyses, the transformation of variables or relaxing the linearity such as restricted cubic splining (RCS) were considered to reflect the data properly and not to violate the model assumptions. When TDT was treated as an ordinal variable, the effects of TDT on CR/CRi and ED were evaluated by Cochran-Armitage trend tests, and the effect on OS was checked by the log-rank test.
Results
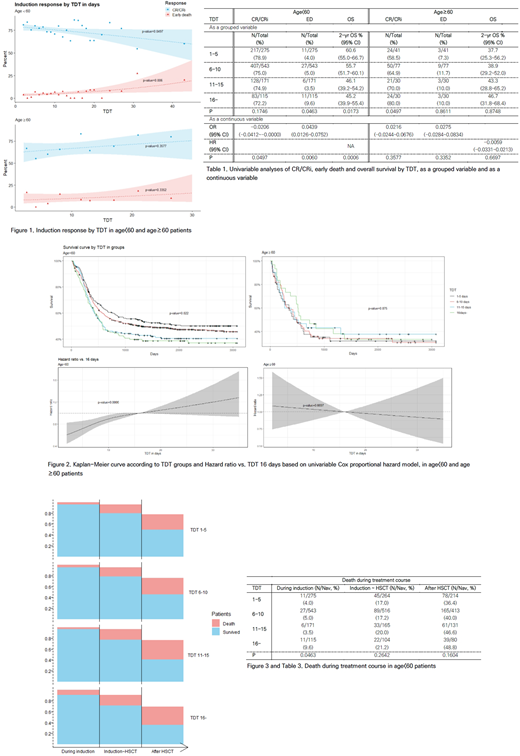
Median age of YG (n=1104) and EG (n=178) were 40 years (interquartile range, IQR; 32-49) and 63 years (IQR; 61-64), respectively. Median TDT of both groups was 8 in days (IQR; 6-11 in YG and 6-13 in EG). When TDT was categorized into 4 groups, patients with higher WBC count tended to belong to earlier TDT groups in both YG and EG cohorts, and secondary AML patients were more placed in the later TDT groups especially in YG cohort. Univariate analyses of TDT in YG showed that TDT had significant correlation with CR/CRi rate, ED rate, and OS. Odds ratio (OR) of CR/CRi per one day treatment delay was -0.0206 (95% CI; -0.0412~-0.0000), and OR of ED per one day delay was 0.0439 (95% CI; 0.0126~0.0752) (Table 1 and Figure 1). RCS method was applied on OS model, so a single value of the hazard ratio (HR) per one day treatment delay was not available, but we could say HR of patients of TDT 2 versus (vs.) patients of TDT 16 was 0.6063 (95% CI; 0.4450-0.8259) in our model (Figure 2). Even after TDT was treated as a grouped variable, TDT was still significant on the ED rate and OS in YG. Especially, High ED rate and low 2-year OS of a group of TDT more than 15 days were noticed (Table 1). In EG, there was no significant effect of TDT on all patients' outcomes (Table 1). Multivariate analyses including age, WBC, AML type, MRC risk, and HSCT status showed that, in YG, TDT effect on CR/CRi rate turned to be insignificant, but TDT still acted as a significant variable for ED and OS. In EG, there was no significant effects of TDT on ED and OS, as like univariate analyses. When the treatment course was divided into 'during induction', 'between induction and HSCT', and 'after HSCT' in YG, there was no significant difference in the rate of death between TDT groups except for the deaths during the induction period (Table 3 and Figure 3).
Conclusion
Our data revealed the effects of TDT on OS and ED in YG, which were significant in multivariate analyses adjusting the effects of other variables. When the timing of death was divided in YG, the only ED was significantly different between TDT groups, especially in the group with more than 15 days of TDT. These results suggest that TDT matters in YG and delayed initiation of treatment over 15 days after diagnosis would increase risk of early mortalities. On the other hand, little effects of TDT on EG provide a rational for sufficient evaluation of comorbidity and functional impairments to select appropriate initial treatment.
Kim:Takeda: Research Funding; ILYANG: Consultancy, Honoraria, Research Funding; Sun Pharma.: Research Funding; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; BMS: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Novartis: Consultancy, Honoraria, Research Funding, Speakers Bureau. Lee:Alexion Pharmaceuticals Inc.: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Kim:Abbvie: Honoraria; Amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Sanofi-Genzyme: Honoraria; SL VaxiGen: Consultancy, Honoraria; Yuhan: Consultancy, Honoraria; AML Global Portal: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Astella: Consultancy, Membership on an entity's Board of Directors or advisory committees; BL&H: Research Funding; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Chugai: Consultancy, Honoraria; Daiichi Sankyo: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Hanmi: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal